[MUSIC PLAYING] Dr. Walsh: Welcome. This is Dr. Kathleen Walsh, a clinical instructor with the Department of Family Medicine at the University of Wisconsin. I’m accompanied by Dr. Melissa Stiles. Hello, Dr. Stiles. Dr. Stiles: Hello, Dr. Walsh, it’s good to be here again. Dr. Walsh: So what are we going to talk about today? Dr. Stiles: We’re going to talk about preoperative evaluation concentrating on assessing cardiac risk. Dr. Walsh: Oh, why is this important? Dr.
Stiles: We know that 25 to 30% of postoperative deaths are from cardiac causes and the rate of postop cardiac events increases with age. So by performing a cardiac risk assessment ahead of time, we can determine who needs further intervention. Dr. Walsh: I think I’m getting chest pain as we speak. How do you assess cardiac risk? Dr. Stiles: I utilize the American College of Cardiology the American Heart Association guidelines which is an algorithm. So there are basically four steps. Number one, have they had any recent revascularization or stress testing, two, you want to determine their clinical predicters, these are underlying disease, signs or symptoms, three, determine their functional capacity, and four, determine surgical risk.
Someone undergoing a breast biopsy, not considered a really high surgical risk. Dr. Walsh: When you say recent revascularization or stress testing, how far back to you go? Dr. Stiles: If a patient has undergone coronary revascularization in the past five years, without worsening symptoms, or patient has had a normal stress test or angiogram in the past two years, without symptoms, they don’t need any further cardiac evaluation, go straight to surgery. Dr. Walsh: What are the clinical predicters? Dr. Stiles: So that’s the next step. So if in the first, they don’t have either, then you need to go ahead and determine the clinical predicters. The clinical predicters are basically history of cardiac disease or are they having any current signs or symptoms. It’s divided into major, intermediate, and minor. So the major clinical predicters are, have they had a recent MI in the past six weeks, do they have unstable angina, decompensated congestive heart failure, significant arrhythmias or severe valvular disease, you want to get a cardiology consult.
Intermediate clinical predicters are, have they had an MI but it’s more than 6 weeks ago, do they have mild stable angina, compensated congestive heart failure or diabetes, then you want to stress test if it’s a high risk procedure or the patient has low functional capacity. Minor clinical predicters are a rhythm other than sinus such as controlled atrial fibrillation, abnormal ECG, such as a frontal branch block, history of a stroke, advanced age, or low functional capacity.
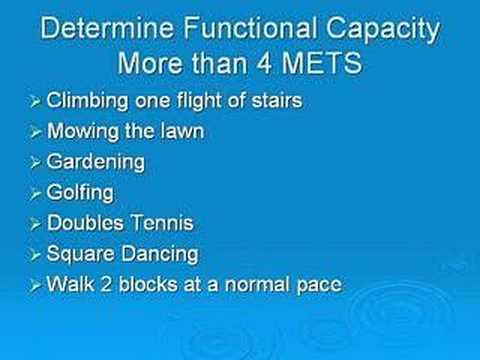
In these people with minor clinical predicters, you want to stress test a high risk procedure and if the patient has low functional capacity, so you need both. Dr. Walsh: How do you determine functional capacity? I mean, if a patient were to come in and they’re pretty active already, they’re mowing the lawn two to three times a week or climbing stairs, or do they have to go through a stress test? I mean, some of them go through stress tests themselves at home. Dr. Stiles: Yeah. That’s a great question. I mean, you really want to make sure they can do at least four amounts, and so the examples you gave are perfect. Can they climb one flight of stairs or mow the lawn? Also, other examples of being able to perform without symptoms are gardening, golfing, playing doubles tennis, or square dancing.
Can they walk two blocks at a normal pace? So if they can do any of these activities without symptoms, then you can be comfortable that they have good functional capacity. Dr. Walsh: How do you stratify surgical risk? Dr. Stiles: Again, we stratify into three different categories, high, intermediate, and low. So a high risk surgical procedure will be one major peripheral vessel, a CABG, anything involving the aorta, prolonged procedure, or emergency surgery. Intermediate surgical risk includes abdominal surgeries, gall bladder, colon resection, thoracic surgeries, head and neck, prostate surgeries, orthopedic procedures, and carotid endarterectomy.
More risk surgical procedures include anything endoscopic involving the eyes, such as a cataract surgery, breast surgery, or other superficial procedures. Dr. Walsh: Can you comment on the role of beta blockers, presurgical, postsurgical or? Dr. Stiles: Yes. They’ve definitely been shown to decrease risk, particularly in patients greater than 65 in the perioperative period, so it’s important, obviously, if they’re on one, you continue it. If they have known coronary artery disease or two or more risk factors for coronary artery disease, you should consider starting one. Dr. Walsh: When do you start it? Like the day before, a week before? Dr. Stiles: Usually start about a week before, and continue then two to three weeks after, and in many patients, you want to consider long term, especially if they have coronary artery disease. Dr. Walsh: I’ve read that those patients who have to undergo emergency surgery, many times you can give a dose of a beta blocker prior to surgery, is that correct? Dr.
Stiles: Yes. There are different protocols. Dr. Walsh: So in review, what are the take-home points? Dr. Stiles: So in review you first want to know if they have had any recent revascularization, stress testing, or angiogram. If not, then focus on their clinical predicters. If they’ve had any of the major clinical predicters, they need further cardiac evaluation. If they have intermediate clinical predicters, then you want to test if they have poor functional status or they’re undergoing a high risk surgery. If they have minor clinical predicters, test if they have poor functional status and they’re undergoing a high risk surgery. Dr. Walsh: Is there an algorithm that we can place into our palm pilot or carry with us to look at if it’s in the morning and I have a emergency surgery I can go through this? Dr. Stiles: Oh, definitely. So just google American College of Cardiology, American Heart Association practice guidelines and you will be able to find this guideline.
Dr. Walsh: Thank you, Dr. Stiles, I appreciate your time. Dr. Stiles: You’re welcome..